It is Not All in Your Head: A Discussion of the Role Lifestyle and Diet Play in Mental Disease
 Nancy A. Palermo MD
Nancy A. Palermo MD
We have always suspected that ultra-processed diets were linked to chronic diseases, including psychiatric diseases like depression and anxiety, but a recently published in JAMA (September 2023) showed that women who consumed the most ultra-processed foods (foods high in salt, sugar, refined carbohydrates, hydrogenated oils, and artificial additives) were 50% more likely to suffer from depression than those women who avoided these foods. This is yet another study to support the fact that mental disorders are not distinct entities and have a tremendous overlap with other physical disorders.
A poor diet can largely influence both mental disorders and physical disorders.
Some researchers, like Dr. Christopher Palmer, a Harvard Psychiatrist and researcher and author of Brain Energy, have even suggested that many mental disorders can be thought of as metabolic disorders of the brain.
Over 800 million people suffer from mental health disorders. This equates to 1 in 10 or 10% of the world’s population. This does not include those individuals with substance use disorders. In the US, these diagnoses are clearly on the rise. In those ages 18-25, there has been a 40% increase in mental disease diagnoses. Women are twice as likely as men to be diagnosed. One in seven women are medicated for depression and anxiety, and 1 out of 4 are on medication by the time they reach their forties.
More disturbing is the rise in autism, which in 2000 was 1 in 150 and in 2014 reported to have increased to 1 in 59. The rising numbers in a short period of time suggest an environmental change rather than a genetic change. We have seen this in medical conditions as well, and the impact on mental disease is no different.
Currently, most diagnoses of mental disorders are based on symptoms. There are no signs or tests used to make these diagnoses. Psychiatry is a field that uses no clinical data or tests to make diagnoses. There is no consideration of root causes when treatment is offered, however, there is sufficient evidence to support that underlying physical disorders can lead to mental symptoms.
New York Times Bestseller Dr. Kelly Brogan, author of “A Mind of Her Own” states, “Depression is not genetic; it is epigenetic”. Our lifestyle has been hijacked, and our bodies and brains are rebelling. Our diet is filled with processed and inflammatory foods; our body lacks exercise and sunlight and is exposed to thousands of chemicals and stressors daily. Many of these triggers may be laying the groundwork for inflammation, nutritional deficiencies, gut inflammation, dysbiosis (microbiome disruption), hormonal changes, and the activation of the HPA (hypothalamic-pituitary-adrenal) axis or stress factors in our bodies – all leading to mental illness.
A growing body of evidence has linked these very disruptions to the development of mental disorders, yet we have been “brain-washed” to believe medication is the answer.
While psychiatric medications have a place, they certainly are not a panacea. They also come with real side effects and withdrawal symptoms and little informed consent and discussion of these. Despite heavy marketing, six decades of research have revealed these medications may not be any better than a placebo and, worse yet, may leave individuals worse off after they stop taking them. There is certainly increasing evidence that we need to look deeper into addressing the root causes to avoid starting medications in the first place.
Let’s explore some of the root causes and contributors to mental disorders. This list is certainly not exhaustive but gives the reader some considerations, separate from medication, in the management of mental disorders.
Medication Induced Mental Disease
There are over 200 commonly prescribed pharmaceutical drugs that list depression and anxiety as side effects, yet few doctors counsel patients on these risks. Many include Beta-blockers, anti-anxiety medications, allergy medications, cholesterol-lower drugs, over-the-counter acid reducers or PPIs, steroids, and yes, even anti-depressants, which have been shown to increase the risk of suicide in users.
Nutritional Deficiencies
Nearly 2/5ths of the population suffer from a severe B12 deficiency, and it is found in 27% of depressed patients. Gut dysbiosis (microbiome disruption), poor digestion, an inflammatory diet, and medications like PPIs have all been linked to the deficiency.
B12 appears to be a powerful antidepressant.
It is believed to be a powerful contributor to methylation in the body and the removal of an inflammatory protein, homocysteine. Methylation is a process that involves the activation of B12 and other substances like folate. Individuals who suffer from genetic methylation defects like MTHFR are more likely to suffer deficiencies and, thus, depression and anxiety. This condition is easily remedied when individuals are supplemented with methylated or activated forms of the B vitamins.
Researchers have also shown a link between declining consumption of omega-3 fatty acids from fish and other sources and an increasing trend in the incidence of major depression. The two omega-3 fatty acids, eicosatetraenoic acid (EPA) converted into docosahexaenoic acid (DHA), have antidepressant effects in humans. In depressed patients’ daily consumption of omega-3 fatty acids in doses of 1.5-2 grams has been associated with mood elevation.
Vitamin D deficiency has become more common due to lack of sunshine exposure and gut dysbiosis. Vitamin D is important for several crucial functions in the body as well as in the brain. Vitamin D promotes healthy brain cells and reduces inflammation in the brain related to memory and cognitive abilities. Low Vitamin D has been linked to Seasonal Affective Disorder (SAD), which is depression associated with the darker months of the year. More severe deficiencies have been associated with depression and panic disorders.
Magnesium deficiency is common in the US due to poor intake of magnesium foods and soil deficient in magnesium due to overfarming. Plus, magnesium levels are inversely related to cortisol levels, so more stress, less magnesium. This can be important when it comes to mental disorders. Magnesium plays a large role in the central nervous system. Magnesium interacts with GABA receptors, supporting the calming effects of the GABA neurotransmitter. Normal magnesium levels in the central nervous system help to counteract the effects of glutamate, an excitatory neurotransmitter.
Individuals with normal magnesium levels in the cerebral spinal fluid are more likely to have normal serotonin levels, and magnesium is needed for dopamine production. All of these roles explain why magnesium deficiencies can support mental disorders.
Thyroid Dysfunction
Thyroid disorders, including both hypothyroidism and hyperthyroidism, may be associated with several neuropsychiatric disorders, including depression and anxiety, yet often individuals go unscreened. Abnormalities include elevated TSH, Low free T4 and T3 levels, and elevations in thyroid autoantibodies. Often, treatment of the thyroid disorder results in improvement or resolution of the associated depression and anxiety.
Gut Disruption and Inflammation
Hippocrates, the third-century Father of Medicine, said, “All disease begins in the gut.”
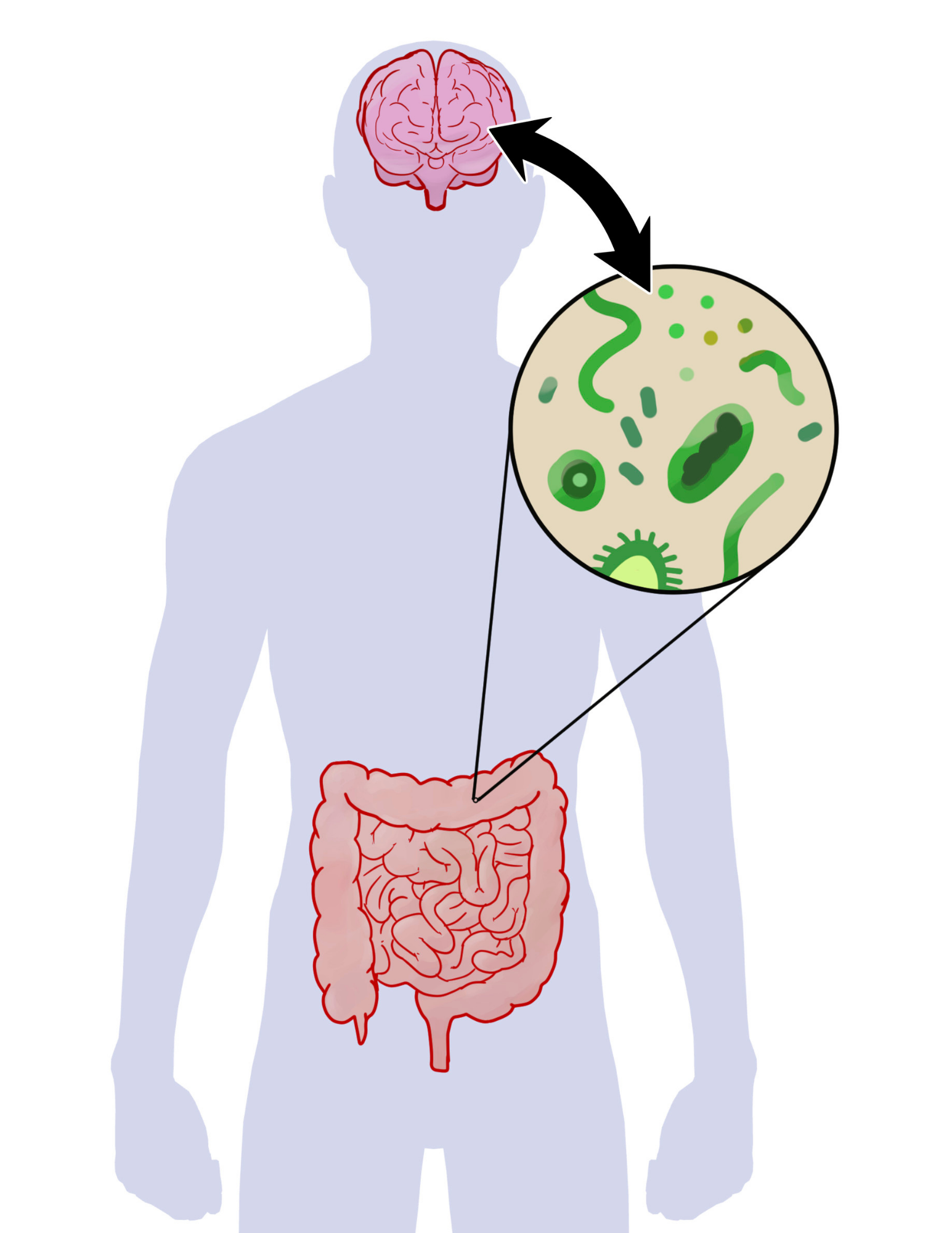
It appears he was correct with respect to many disease states but possibly to mental disease as well. Several studies have linked the role of gut dysfunction in inflammatory conditions that directly affect the brain. The Vagus nerve is the longest-running nerve and connects the brain and the gut. The gut-brain axis appears to be bidirectional through the Vagus nerve, the immune system, and the neuroendocrine system (HPA axis).
Many of us know first-hand the gut-brain link when we experience distress felt as stomach upset or butterflies. It appears that inflammation in the gut can also trigger such reactions in the brain. Inflammation in the gut caused by infections, highly processed foods, as well as allergenic foods like gluten, dairy, sugars, and additives appear to cause higher levels of inflammatory markers in the blood, which can lead to depression.
It appears these markers directly relate to the level of depression as well – higher levels of inflammatory markers are associated with more severe depression and anxiety. Some conditions, like Celiac disease, which are associated with such markers as well as significant inflammation in the gut, often present as psychiatric disorders first. Anxiety and depression are common presenting symptoms of Celiac disease.
Our microbiome, the trillions of bacteria that reside in our gut, is also essential for healthy brain function.
Researchers have revealed certain types of bacterium types may be associated with anxiety and depression. Researchers in the Netherlands found that strains like Coprococcus and Dialister were severely deficient or absent in depressed patients. These bacteria are believed to be involved in the pathway to produce Dopamine, our feel-good neurotransmitter, and are sources of butyrate production, a potent anti-inflammatory substance.
Probiotics have demonstrated antidepressant effects in clinical research studies. Fecal Microbiota Transplant (FMT) is a procedure where a healthy donor’s fecal microbiota is transferred to an unhealthy recipient. FMT has been used to treat severe gastrointestinal infections like C. Difficile. Recently, in a small study, FMT has been successfully used to treat individuals with severe depression and anxiety. The success of fecal transplants in treating severe depression further supports the microbiome’s role in mental health.
Blue Light Exposure and Reduced Sleep
“We need rested warriors.” Cunningham
Our society is on 24-7.
We go nonstop and feel we must keep working to get everything done. Then, we spend the remainder of our time on social media or watching TV, further exposing our brains to blue light. Being exposed to blue light well into the night can have a profound impact on our sleep. One in three Americans do not get enough sleep, and 60% say they have trouble sleeping most nights. Sleep disruption is related to our high-stress, light-infused, sedentary lifestyle, and it seems to be worsening our mental health.
Reduced sleep is associated with a 4 times increase in depression, a doubling of anxiety risk, and four times the risk of developing drug or alcohol abuse. Lifestyle habits that prioritize sleep can have a profound impact on mental disorders.
Disruption of GABA Neurotransmitter
GABA is one of our neurotransmitters. It is the chief inhibitory neurotransmitter in the developmentally mature mammalian central nervous system. Its principal role is reducing neuronal excitability throughout the nervous system. It is then a calming neurotransmitter. Our daily habits can inhibit or compromise GABA’s production and role. These habits include alcohol intake, prolonged daily stress, whether real or perceived, poor nutrition and glucose dysregulation, benzodiazepine use, and gut dysbiosis.
Social Media: The Silent Killer of Your Mental Health
Social media and technology can be powerful tools to interact and share ideas. At its core, it is beneficial.
Unfortunately, it has been designed to sabotage our attention. We all know that, often, once we start scrolling through social media, we cannot stop. The algorithm of its development favors anxiety. It is media overload, and your attention is a commodity, so they will use whatever tactics they can to keep you on it.
Unfortunately, mental health is collateral damage.
Many studies have shown an increase in mental health diagnoses with the advent of social media. This is especially prevalent in teens. A 2019 study suggested that teenagers who use social media for more than 3 hours daily are more likely to experience mental health problems, such as depression, anxiety, aggression, and antisocial behavior.
The use has only increased since the pandemic. Unfortunately, a study reported earlier this month showed use amounts to 4.8 hours per day for the average U.S. teen across seven social media platforms tested in the survey. Across age groups, the average time spent on social media ranges from as low as 4.1 hours per day for 13-year-olds to 5.8 hours per day for 17-year-olds. This alone could explain the significant increase in the incidence of mental diagnoses in teens.
While this discussion may seem overwhelming, it is simplistic because it supports the idea that our environment can affect our health. It is ammunition to support the belief that medication is not the only solution. With many chronic medical conditions, we now understand the role our diet, habits, and mindset can play. These things are within our control if we make them a priority. While medication may be a necessary intervention, at least temporarily, we must put equal emphasis on the roles diet and lifestyle play on our mental health and our overall health.
Join me in this month’s Yoga and Learn, where we will discuss the topic of contributors to mental disorders and develop a checklist to help you ensure you are addressing these factors.



